Health Centre for Gender and Sexuality (HKS)
Oslo Municipality’s Public Health Centre for Gender and Sexuality (HKS) has developed an innovative service for clinical health support to transgender and gender diverse persons. Here you can read more about who we are, how we work, who we are for, our history and our goals.
The health centre delivers a city-wide health service in the Norwegian capital for the municipality's residents between the ages of 0-30.
Our mandate is to reduce health gaps between minority and majority groups related to gender and sexual diversity.
The service is free of charge, confidential and low-threshold. Low-threshold means that you do not need a referral to get in touch with us, just send us an email directly.
Services we provide
Psychosocial therapy: We provide individual therapy sessions focussing on gender identity, sexual identity, and sexuality. Our consultations are tailored to your needs, helping you find the best support together. Examples: exploring and reflecting on sexuality, sexual identity, or gender expression; stress management; support during coming out; preparation and assistance with psychological, social, or sexual changes during a gender transition; exposure therapy through meetings outside the clinic.
Family or couples councelling: Depending on topics, age and needs, we involve caretakers and/or partners in therapy.
Group interventions: We organize group sessions for transgender people with different therapeutic focus.
Assessment: A thorough assessment of gender incongruence in the event of a need for referrals to other healthcare providers and/or medical gender-affirming treatment.
Medical treatment: For people with gender incongruence, gynecological exams, puberty-blocking treatments, and hormone therapy are available after individual assessments. These assessments includes discussions about gender incongruence, psychological, social, and sexual aspects of transitioning, potential future regrets or detransitioning, and the effects and side effects of medication. The process is tailored to each person's age, needs, and preferences.
Gender-affirming prosthetics and other aids: Referral to the appropriate branch of the healthcare system in other to obtain prosthetics and other aids.
Collaboration with specialist health services as needed. For clients under 18 years old we work together with families, and when necessary or desried, we may cooperate with our young clients’ schools.
A unique service in Norway
HKS is a specialized low-threshold service that provides broad sexual health support through interdisciplinary expertise, to residents of Oslo.
HKS emphasizes interdisciplinary collaboration to enhance resilience through normalization and de-pathologization. Our main activity is the therapy provided by our interdisciplinary team, where everyone has either additional accredited education in sexology or trans health. We are open to explore new ideas to meet client needs, and have over the last couple of years tried for example efforts such as art therapy groups, social exposure therapy for clients facing challenges like shopping for gendered wardrobes, or psychomotor physiotherapy.
Most clients seeking out the clinic today are trans and gender diverse individuals. The health center provides services for clients to explore their gender identity, including counseling, family therapy, group meetings, as well as hormone treatment. For clients with complex needs, we refer to and cooperate with specialists in order to offer complete care.
We help individuals aged 0-30, supporting them through changing requirements from childhood to adulthood as needed.
The team
Our clinical team currently includes psychologists, pediatric and public health nurses, social disability nurse/workers, family therapists, and psychotherapists, all trained in sexology and certified by the Nordic Association for Clinical Sexology.
The team also includes an endocrinologist specialized in transgender health and general physicians, overseeing hormone therapy on a daily basis, based on guidelines from The Endocrine Society.
HKS values interdisciplinarity, sexology, trans competence and variety of lived experiences when putting together our team.
You may read more about each member of the team further down.
Our model:
Free public health clinic for gender and sexuality
Strengthening primary healthcare
Low threshold – no referral required
Sexologically grounded clinical service
Adherent to definitions and standards in ICD-11, SOC8 and The Endocrine Society
Joint decision making leaning towards informed consent
Care across life phases (0-30 years)
Building resilience through normalization and innovation
Comprehensive, individualized care
Cooperation with patient organisations and health care providers across sectors
Strengthening competence through keeping up to date with medical advances, and remaining open, curious and innovative in our clinical practice
Our background
The clinic has evolved over time to address healthcare gaps for TGD individuals in Norway. Opened in 2002 as the Public Health Centre for LGB Youth (later LGBT Youth), initially a public health nurse and a doctor shared a part-time role, assisting young people discussing their queer sexuality, often for the first time.
Over the years, the client group shifted towards more trans and gender diverse individuals, prompting the clinic to adapt to the more complex needs of this group.
In the past decade, HKS staff has grown and diversified, making sexological training mandatory for therapists. The name change to Public Health Centre for Gender and Sexuality (HKS) followed, highlighting a new understanding about the diversity of human sexual and gender experiences.
Why sexologists and what is sexology?
The word "sex" in English refers to both physical sex and sexuality more broadly, and sexual health is connected to both body function and mental health. Accredited sexological education offers knowledge about the body and mental health, about diverse genders and sexualities, gender identity, sexual identity, minority stress, and natural diversity among human beings. Gender incongruence is included in the chapter on conditions related to sexual health in the international diagnostic manual ICD-11 (WHO 2018), and sexual health is an important aspect of gender transition. Sexology naturally holds an important role in gender-affirming care.
Certified sexologists from the NACS (Nordic Association for Clinical Sexology) have a professional background in health or health-and-social care, along with additional training in sexology. The certification demands proof of supervised therapy practice. Discussions about sexuality and gender can trigger strong personal feelings, both positive and negative. As part of their training, sexological therapists learn to actively reflect on their own attitudes, reactions, and feelings, as these may appear in and impact therapy setting.
How HKS supports clients with gender incongruence
HKS has a trained team that works with TGD individuals and follows the Norwegian health guidelines to ensure healthcare for those with gender incongruence is available and nearby (following the so called LEON principle = Lowest Effective Level of Care).
Guidelines for supporting trans and gender diverse (TGD) individuals
Our approach at HKS follows national and international guidelines:
The International Classification of Disease, 11th revision (ICD-11) by the World Health Organization (WHO)
Recommendations from the World Professional Association for Transgender Health (WPATH) in the Standards of Care for TGD individuals, 8th version (SOC8, issued in 2022), which are based on extensive clinical experience and research, and a transparent method for development of recommendations
The above documents form the evidence base in the National Norwegian Healthcare Guidelines for Gender Incongruence, issued by the Norwegian Directorate of Health, which focuses on the organization of healthcare delivery rather than clinical practice.
Individualized follow-up
We have an increasing demand and unfortunately an increasingly longer queue before the first appointment with us. After the first session we will set up new conversation sessions about every 3 weeks. We have no requirements for a certain number of sessions per client, as each person's needs are so different. Working together with our clients, we provide individualized care as long as they require it.
Clients are followed up by a main therapist who gets to know them well. Therapists also collaborate with other members of the team during the course of follow up - either through inviting colleagues to therapy sessions, or discussions in bi-weekly interdisciplinary teams.
Clients who experience gender incongruence, our largest client group, have needs that can vary and develop over time. There are about 3 weeks between meetings in the beginning when needed, and in the most active psychosocial assessment/follow-up phase, later meetings can be requested if new issues arise.
In cases of trans and gender diverse youth
Younger users of HKS services primarily access HKS on basis of gender identity questions. They are often supported over many years. Parents are usually involved and sometimes we are invited to participate in school meetings or information meetings in clients’ classrooms.
Only a few of our clients under 18 opt for any form of medical treatment. Some wish to wait, others don’t need it. See our statistics section further down for more information on the numbers.
We cooperate with child psychiatric services and school health services as needed.
In cases of trans and gender diverse adults
In adult clients, in the age group 18-30 years old, therapeutic questions vary, covering sexual orientation, sexuality, and gender, with many clients needing follow-up at different levels. However, even in the adult group, gender incongruence is by far the most common reason for why someone contacts HKS.
HKS will cooperate with other services as needed. While many contact HKS because they wish to access gender affirming medical interventions, the majority - even among TGD individuals - have other needs and questions they wish to work through with our therapists.
Therapy themes may include:
Clarifying thoughts on gender and body
Educating on various aspects of gender
Family and couples therapy
Improving family communication
Connecting with like-minded individuals
Enhancing communication in school/work place
Managing minority stress, shame, body dysphoria, and mild anxiety/depression
Practical support for aids, clothing, and makeup
Provide information about issues connected to body image, relationships, and sexuality before, during or after a gender transition
Information on medical treatment options and access
Transition follow-up
Referrals

Medical interventions at HKS
Hormone therapy and puberty blockers
Expertise in hormone therapy
HKS has specialists in hormone therapy, led by an endocrinologist (hormone doctor) who specialises in gender affirming hormone therapy and serve as a mentor within the related WPATH education programme. We adhere to international definitions and guidelines from the Endocrine Society, as well as those mentioned earlier from WPATH (SOC8), WHO (ICD-11), as well as the Norwegian Directorate of Health's overarching national standards.
Exploration, assesments, information sharing and decision making
Everyone who seeks gender affirming hormone treatment at HKS first speaks with a sexological therapist, discussing in depth personal and social perspectives on, and experiences with, sex and gender. We also further have conversations about effects, side effects and common reactions not only to the medication, but also to the transition process, including biological, social, psychological and sexual factors. We always discuss potential treatment dissatisfaction, and ask clients to reflect on how they might handle possible future regrets or change in gender identity.
Our goal is to create a mutual trust to facilitate a process of reciprocal information sharing and understanding. We want to enable the client to “turn every stone” that may be relevant to “look under”, in order for each individual to reach an informed decision about social and medical transition. The process and number of meetings required therefore vary from person to person. As our doctors also has a long waiting list, we strive to use this waiting time wisely, offering the best of our knowledge, advice and challenging preconceived notions as needed.
Caretakers are involved for clients under 18 according to guidelines, and family or partners are welcomed to join for older clients.
Hormone treatment routines
The hormone treatment schedules follow international standards. We have developped internal routines adapted to the Norwegian circumstances, based on guidelines from The Endocrine Society. We usually start up with low doses and gradually increase, monitoring the effects every 4-6 weeks in the initial phase, reviewing blood tests and discussing with patients physical and mental experiences of treatment, before making adjustments.
Psychosocial support is offered during this phase. Once satisfactory hormone doses are achieved, the follow-up will be less frequent, and the medical treatment is eventually transferred to the clients’ family doctor, with whom we cooperate as needed. Psychosocial support may continue on a less regular basis up until 30 years of age. Due to restrictions in capacity, any need for deeper theraputical interventions are reffered to psychatric services, with our cooperation if warranted.
Gynaecological examinations
As of September 2023, we offer gynaecological exams for transmasculine individuals, as well as check-ups for transfeminine patients.
Our experiences and results as related to our goals
Accessible: Being able to contact the clinic directly reduces waiting times and potential for gatekeeping; this makes the service accessible to all. Increasing demand and limiting jurisdiction (Oslo only) and age limit, restricts the accessibility of the service.
Individualised: Each client has a different pathway “through” the clinic, and the clients’ needs and experiences are discussed at every meeting point.
Comprehensive: Following clients through many life stages, the clinic can provide different kinds of support at different stages, with a variety of possible interventions. Drawing on the competencies of a multidisciplinary team, and remaining open to innovation, we may assist a variety of needs. For those needing more complex or specialised care, we strive to cooperate with other health care providers. Increasing demand and waiting times however forces the clinic to make some hard priorities in the services we provide.
De-stigmatizing: The centre has developed outside hospital and psychiatric settings, and has a main focus on resources, diversity and positive markers for health.
Competent: Sexology provides specific competence on sex, gender and minority identities. Cooperation with patient organisations, the clients themselves, and taking part in WPATH and other arenas for professional discussions and following the latest clinical guidelines and research are integral to how the clinic has developed.
Providing relief: We have initiated cooperation with the University of Agder to do rearch on the short- and long-term consequences of the care provided at the centre. Our experience today is that patient organisations and the patients themselves report satsifaction, and health personnel that reach out for our support report that they find our services helpful. We would however like to see more rigorous research into the successes and shortcomings of the service. We hope independent researchers will conduct a long-term study on the client groups receiving support in various clinic models for healthcare delivery to the TGD group in Norway, allowing us to learn from one another and grow further.
Results in numbers
Norway is a small country of 5 million people. Oslo has around 700 000 citizens as the capital and largest city. We include here some statistics from our clinic, which services Oslo’s population under 30 years old.
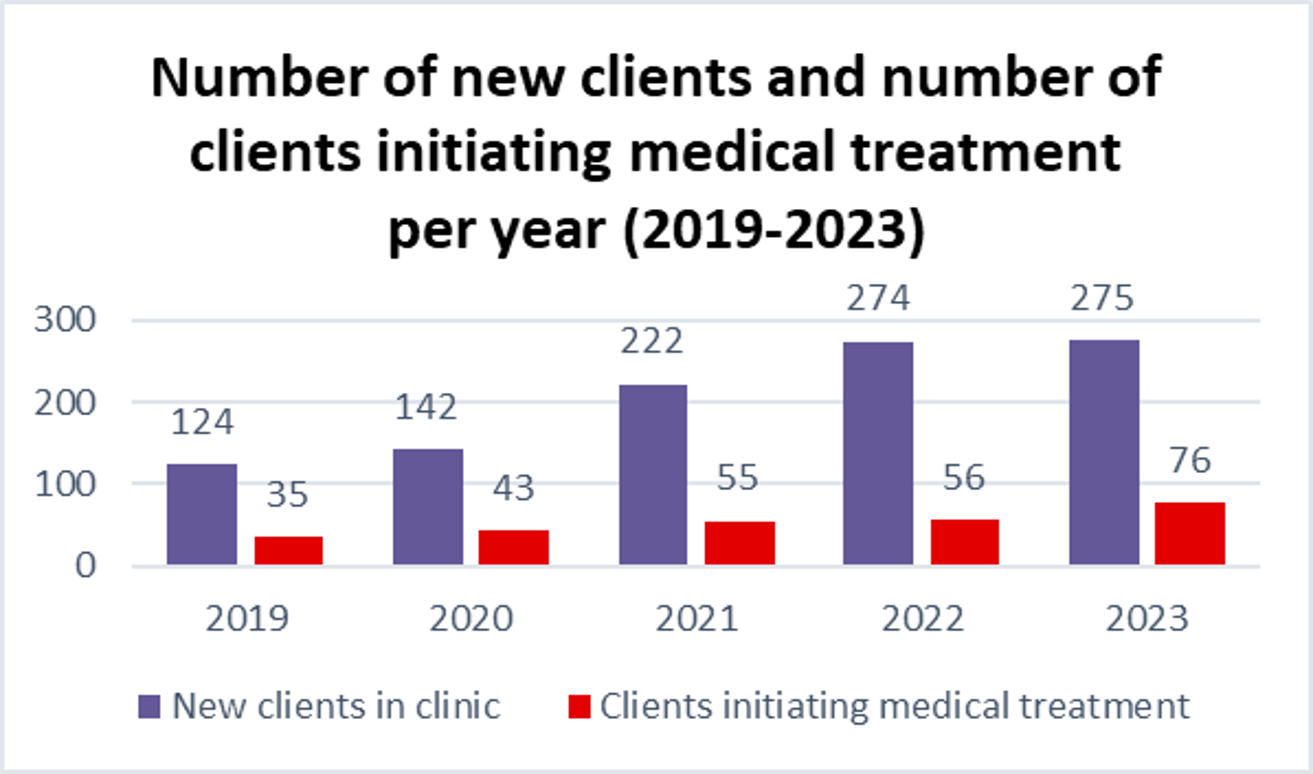
Table 1
The clinic has seen a steady increase in demand over the last decade.
The increase cannot just be explained by the general inrease in demand for gender affiring healthcare, that has been seen all over the world in the same time period. The clinic has changed a lot in its provision of care in the same time period. In the last years media has written about it, so it has become more renouned.
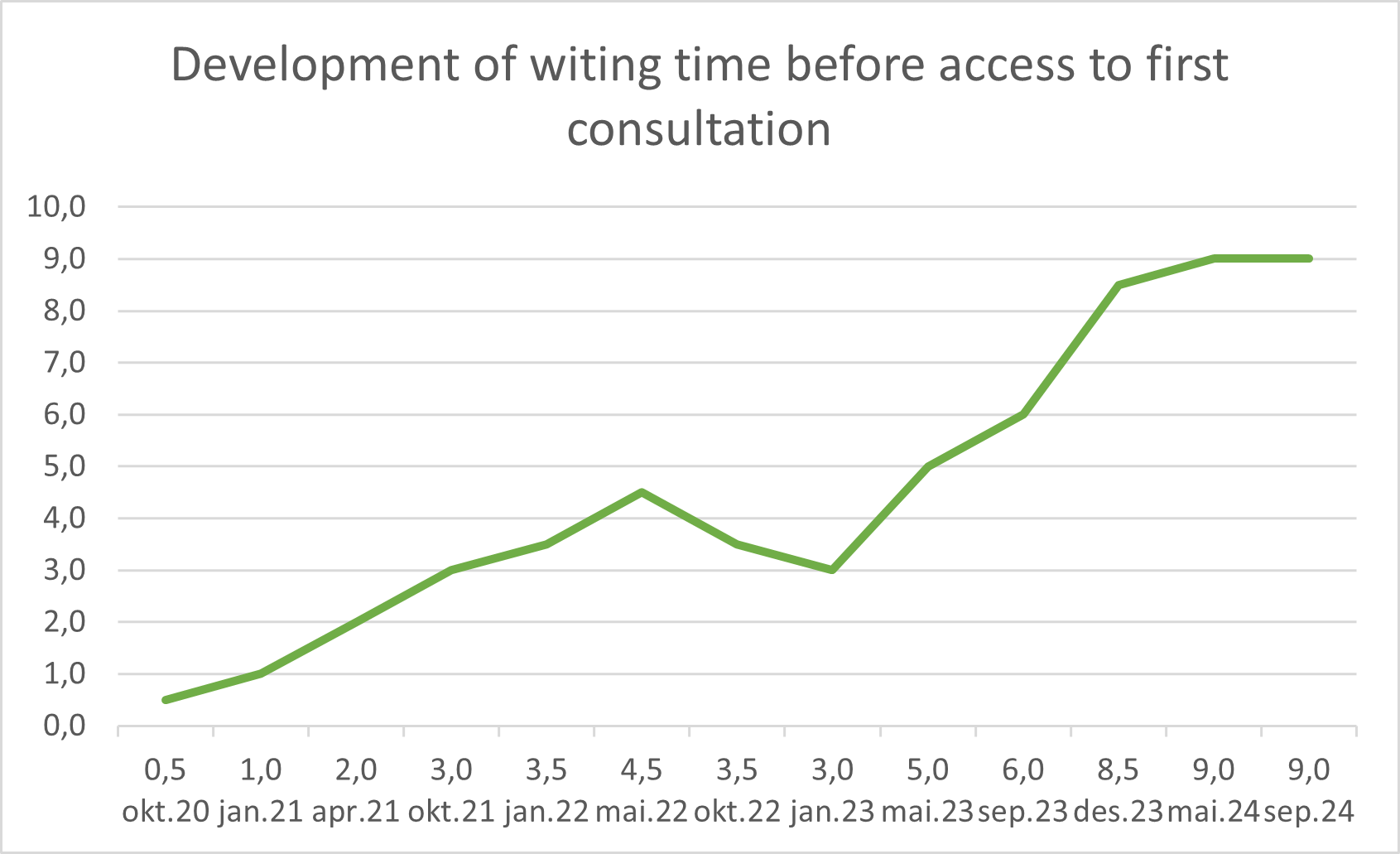
Table 2
Waiting lists and times have lengthened due to increased demand. Initially, we expanded staff. A stable funding combined with temporarily reduced capacity over the last year have hindered increase in intake. We are hopeful that staff capacity will increase next year, preventing further delays, and perhaps even shortening the waiting times.
Table 3
Clients under 18 years old are prioritised at the clinic. An example of this is that the waiting time is cut to maximum two months for the youngest clients. This is possible as long as they remain under a third of our client group (n=47). The majority of new clients in 2023 (n=113) were between 18-24 years old, with individuals between 25-30 years old were almost the same number (n=108).
Table 4
This table indicates that most clients at HKS do not use our medical services. We have increased the clinic's medical doctor capacity significantly over the last years. Clients who start medical treatment typically have been visiting the clinic for several months or even years beforehand. Each person's path to medical care varies but follows our guidelines.
Table 5
Transmasculine individuals (ascribed female at birth, AFAB) lead medical care demand under 18, but transfeminine clients (ascribed male at birth, AMAB) surpass AFABs in following age groups.
This suggests that increase in adolescent AFABs seeking gender-affirming care nationally over the last 10 years, may relate to well known factors such as a heightened stigma on social boys expressing any kind of femininity during their high school years.
Table 6
The trends seen in Table 5 for 2023 are consistent over time.
Table 7 and 8 below
The trends seen in Table 6 is consistent with numbers from the central Norwegian National Centre for Gender Incongruence.
The first table shows gender ratio of all those who transisioned medically in our clinic in the years from 2019 and 2023, which correspond more or less to all those seeking medical transition at the clinic. The second table shows all those reffered to The National Centre for Gender Incongruence for 2022. The National Centre is the only other public health service which provides gender affirming medical care in Norway. The centre does not provide psychosocial gender support, exploration, etc; their stated role is to screen for eligibility and provide medical gender affirming care. This entails that more or less all those who are reffered there from out-patient psychiatric centres or newly established regional centres for gender incongruence, seek medical transition.
Neither HKS nor the national centre provide comparable numbers broken down to gender and age groups for the years before 2019. We have found numbers for the gender of all referrals to the KID team (under 18 unit) at the national center since 2002 until today. However, as we attempt to show here, numbers for legal minors shown separately from adults, only tells half the story and may lead to some assumptions that are not supported by the other half of the story.
Other activities at HKS
Training health professionals
HKS offers courses for health care workers. Our team can tailor lectures and programs to suit different needs. We invite health care workers to visit or intern at our clinic.
iChatten.no
iChatten.no began in 2019 by the Health Centre for Gender and Sexuality (HKS) in response to many requests from people and health workers across the country. We saw the need for a dependable national service for advice and support.
Spør først! (Ask first!)
Ask first! (Spør først!) is an educational program for primary, secondary, and upper secondary schools aimed at preventing sexual abuse and encouraging healthy sexuality. It is connected to school health services and aligned with school curricula.
Conference 2024
In spring 2024, HKS held a conference on neurodiversity and gender incongruence in youth. Speakers included Scott Liebowitz, child psychiatrist; James Byrne, psychotherapist focused on neurodiversity and LGBT+; Ole-Petter Hamnvik, Boston endocrinologist and Harvard professor (replacing Gary Butler, child endocrinologist from England); Lene Løvdal, human rights lawyer; and Vesle Krey, neurodiversity activist and scholar.
Translating the SOC8
HKS financed and organised the translation of the Standards of Care for the Health of Transgender and Gender Diverse People, version 8 into Norwegian. The guidelines were developped by the World Professional Association for Transgender Health (WPATH) in 2022, following rigorous processes that you can read more about on their homepage.
Poster presented at the WPATH conference 2024
At the annual conference of the World Professional Association for Transgender Health 2024, we showcased our clinic to clinicians and researchers internationally. The aim was to present an example of how to organize health services to better support our target communities in various social contexts, and we invite anyone interested to explore this model to contact us.
We provide accessible, individualised, comprehensive, destigmatizing gender-affirming care including some medical interventions, with the aim of providing relief and support clients in developing strengths. We also provide education in order to improve healthcare provider competency in this field across the rest of Norway, where comprehensive low threshold services are less available.
The clinic has evolved to its current form in response to healthcare gaps for transgender and gender diverse (TGD) individuals coming to our health centre. Currently, some TGD young adults and families relocate to Oslo in order to access our services. Not unexpectedly, HKS faces some public controversy as transgender youth healthcare is debated in Norway and globally. The national patient organisation has surveyed their members, who report high satisfaction with care received at the clinic.
Our experience is that a low-threshold sexological clinic like HKS could provide a model for achieving positive outcomes, through meeting diversity in a holistic way, as a viable alternative to traditional clinics in psychiatric hospital settings. We hope for opportunities to explore this with clinicians and researchers in the time to come.
You can view the poster by clicking on the image above.
Who’s who at HKS?
Meet therapists with at least 60 university credits in sexology and supervised practice. They understand body diversity, relationships, sexuality, gender identity, gender incongruence, sexual orientation, and identity. Confidentiality is ensured.
Ingun Wik
Head of Department HKS, Public Health Nurse, Paediatric Nurse, Clinical Sexologist (NACS), Psychotherapist (EFDA). Ingun has worked at HKS since 2012 after several years at a hospital paediatric oncology department.
Tone B. Aanderaa
Public Health Nurse, Clinical Sexologist (NACS). Tone worked as a public health nurse in Oslo. She leads the national project Ask First!, which teaches teenagers about setting boundaries and positive sexuality.
Petter Winther-Brose
Social Educator-Nurse, Clinical Sexologist (NACS). Petter’s background is with individuals with developmental disabilities as well as in acute psychiatric care. He is the leader of the Norwegian Association for Clinical Sexology.
Yon Galezo Cardenas
Specialist in Psychology and Specialist in Sexological Counselling (NACS). Yon specialises in clinical habilitation for developmental disorders, having many years of experience from A-hus hospital. He has practiced in Colombia and South Africa.
Thea Grepperud
Thea is a psychologist and is training to be a sex counselor. She has experience at Public Psychiatric Health Centre, student health services, and outreach youth work with the FACT team. She has interned in a Youth Psychological Centre in South Africa.
Noah Skullestad
Psychologist. Noah has experience from a Public Child and Youth Psychiatric Center and an acute psychiatric unit. He wrote his final research paper on treating anorexia.
Kristine Egeberg
Family therapist, social health nurse, and sexological counselor specializing in gender and sexual diversity. Kristine has long experience with Family Welfare service.
Ole-Petter Hamnvik
Endocrinologist. Ole-Petter is an associate professor at Harvard Medical School, and works at a gender clinic providing gender-affirming care at Brigham and Women’s Hospital, when he is not assisting HKS team.
Jason Lund
Assistant physician. Jason is a general doctor who has worked as a family doctor in Norway. He is getting certified in gender-affirming treatment through WPATH.
Linde Steenvoorden
Assistant physician
Linde is a doctor with a personal commitment to trans health that has brought her to lend her services to HKS.
Cecilie Nordfeldt
Communication and Management Support
Cecilie is a trained social anthropologist who has researched women's health and social change in India. She has extensive experience in project work.
Marie Rist Forsmo
Consultant, Coordinator
Marie has a degree in literary studies, with gender studies as a supporting subject. She is a racer at organisation and systematisation.
“When you show up as your authentic self, whatever that may be, you allow others to do the same, creating the world we all deserve.”
Shanna Katz Kattari (they/them) professor, sexuality educator and activist